Image above: Some of the UMMC researchers teaming up with scientists at Harvard and MIT to study the early cellular response to COVID-19 and what it may tell us about the progression of the disease include, from left, Yilianys Pride, Haley Williams, Dr. Tanya Robinson, Dr. Anna Owings, Hannah Laird, Taylor Christian and Dr. Sarah Glover.
Some people infected with SARS-CoV-2, the virus that causes COVID-19, experience few symptoms, while others develop disease that leads to hospitalization, mechanical ventilation, or even death.

Researchers at the University of Mississippi Medical Center worked with a multi-institution team to get closer to that answer. Published online July 23 in the journal Cell, the paper shows how the response of different nasal cells to the early stages of infection may predict the progression of COVID-19.
The finding could be life-changing for people who are headed toward a severe case of the virus.
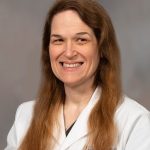
Dr. Sarah Glover, professor of medicine and director of the Division of Digestive Diseases, led the UMMC-based portion of the work in collaboration with researchers at the Ragon Institute of Massachusetts General Hospital, the Broad Institute, the Massachusetts Institute of Technology, and Boston Children’s Hospital/Harvard University. Fourteen of the paper’s 25 co-authors come from UMMC, including School of Medicine faculty, trainees, and research and clinical staff.
“The nasopharynx is an entry point for understanding immunology for COVID-19,” Glover said. The nasopharynx is the area where the nasal cavity meets the throat. Because COVID-19 is a respiratory illness, it’s where viral particles first enter and colonize the body. It’s also the spot health care workers target when they take a swab sample to test for the disease.
The abundance and availability of nasal swabs presents a “way to study the mucosal immunology in COVID-19 patients without being overly invasive,” she said.
Glover and her colleagues gathered 58 swabs from UMMC adult patients, including 35 with confirmed COVID-19 ranging from mild to severe. As controls, they also collected 17 samples from healthy volunteers and six from patients with respiratory failure not caused by COVID-19.
Scientists at the Broad Institute used genetic sequencing technology to identify different nasopharynx cell types from the swabs. They studied the cells’ RNA, the molecules that translate DNA’s instructions into protein’s functions. This allows the scientists to see a snapshot of each single cell’s response to SARS-CoV-2 during the early stage of infection.
The study found that people who went on to develop mild or moderate COVID-19 symptoms had cells with a stronger anti-viral immune response than people who developed severe disease. This happened even though the two groups had similar viral loads and similar health statuses prior to COVID-19.
Glover said she was surprised by the importance of the epithelium, the surface-layer cells that serve as the body’s first line of defense against infections, in determining what path a patient’s disease may take.
“This virus causes significant distortion of the innate immune system,” Glover said, adding that SARS-CoV2 “changed the makeup of the cells in the nasopharynx of people with severe disease.”
Among COVID-19 patients, they found more mucus-producing secretory cells and fewer particle-filtering ciliated cells. They also found that patients with severe COVID-19 had more macrophages, the immune cells that help lead to the cytokine storm often seen in serious cases. Another part of the study showed that SARS-CoV-2 targets particular kinds of cells.
“Our findings suggest that the course of severe COVID-19 may be determined by the body’s intrinsic antiviral response to initial infection, opening up new avenues for early interventions that could prevent severe disease,” said Dr. José Ordovás-Montañés, co-senior author and assistant professor at Harvard Medical School, in a Broad Institute news release.
The samples in this study came from patients treated between April and September 2020, encompassing the first wave of Mississippi cases. Glover and colleagues are working on a follow-up study to compare these initial findings to patients with Delta-variant COVID-19 or breakthrough infections post-vaccination.
The Glover lab at UMMC focuses on immune system-associated GI conditions, such as inflammatory bowel disease. Researchers started working on COVID-19 and immunity with Dr. Bruce Horwitz, a pediatric emergency medicine physician at Boston Children’s Hospital and one of the paper’s senior co-authors. Since 2019, Glover and Horwitz had been looking to collaborate on immunology-based research. When COVID-19 emerged, they quickly mobilized to assemble a team.
“We were very excited when Dr. Glover approached us with an idea to perform this research. Dr. (George Abraham, UMMC professor of medicine) and I were identifying the patients and enrolling them in the study. The results stress out the importance of epithelial immunity and help us better understand its response to SARS-CoV-2,” said Dr. Michal Senitko, UMMC assistant professor of medicine. Both pulmonologists are co-authors on the study.
The UMMC co-authors also include Dr. Anna Owings, a chief resident in internal medicine. She conducted research in Glover’s lab before COVID-19 and worked in the intensive care unit that cared for COVID-19 patients in 2020.
One of her roles in the study was to monitor participants’ health charts during their time in UMMC, which allowed researchers to correlate their health outcomes with the cellular and RNA-level data coming from the laboratory.
“At that time, we were serving so many COVID-19 patients and wanted to expand the knowledge because we didn’t know much and were trying to figure out how we can help our patients,” Owings said, adding that it was powerful to “see everyone come together to work toward a common goal: to protect humankind.”
As with any human-subjects study, Owings and Glover say, the work would not have been possible without the patients and their families who volunteered for the research. The results of this study will help other patients with not only SARS-CoV-2, but also other respiratory diseases.
“This research opens up a lot of doors in understanding how the nasopharynx modulates our response to viruses and other infections,” Glover said.
Funding for this project came from the Chan Zuckerberg Initiative, the National Institutes of Health, New York Stem Cell Foundation, Richard and Susan Smith Family Foundation, AGA Research Foundation, Food Allergy Science Initiative, The Leona M. and Harry B. Helmsley Charitable Trust, Crohn’s and Colitis Foundation, and Bill and Melinda Gates Foundation.
Story provided by Karen Bascom, University of Mississippi Medical Center Office of Communications and Marketing